COVID Updates for 02-16-21
We are all learning, and by “we,” I mean thinking people. Lots of intelligent questions from the February newsletter, as well as some important new research. Here are the most common issues.
-
There are now 3 new mutated strains of the SARS-CoV-2 virus. Some research suggests that the Moderna and Pfizer vaccines are not as effective against these strains, so what now?
Stephen reply:
Ever since I watched T-cells cloning right before my eyes with my first 400x microscope, I have been in awe of the human immune system. I mention that because I want to get away from the “only vaccines can save us” mindset. Point being that brilliant immunologists will continue to tweak the vaccines, but the best hope to remain healthy is by supporting your immune system, which can adapt to pathogens a lot faster (and in many ways better) than any vaccine.
Action Steps
- You should have our Four Stages of Infection tacked to your wall. DOWNLOAD
- Note that we’ve added Turkey Tail concentrate to MMIS. ORDER HERE
—–
-
There is still widespread confusion regarding herd immunity
Dr. Natalie reply:
This issue is confusing because policy-makers continue to make unscientific statements, equating mass vaccination with herd immunity and the end of the pandemic. There are a dozen reasons why this is not going to happen, and importantly, it doesn’t have to.
- Only once has mass immunization against a virus produced herd immunity. Polio was a remarkable success but bears no resemblance to the current situation.
- Polls find that from 25 to 35% of Americans are unwilling to be vaccinated, and there are legitimate reasons for making that decision.
- Even if 70% of Americans are vaccinated, with modern levels of global travel, the herd immunity goal is next to impossible.
- Stephen and I believe that the Covid-19 vaccine is rightfully intended for the vulnerable, very much like the flu vaccine. Forget herd immunity. The goal should be reducing hospitalizations and deaths by mitigating the severity of the infection. The Covid-19 vaccine can do that without targeting 70% of the world population.
Action Steps
- Keep your immune system strong and reduce risk as much as possible. In addition to our nutritional recommendations, make sure you are exercising regularly, getting adequate sleep and managing stress. Check in with with family and friends to offer and receive support. “Community builds immunity.”
- As noted in our Four Stages of Infection chart, DHEA plays a critical role in all four stages. High levels of DHEA are associated with stronger mucosal immunity (ie in the nose, mouth and throat) and thus may have value in reducing the rate of infection. If you do become infected, DHEA acts as an immune modulator to reduce the risk of hyper-inflammation.
- Unfortunately, vaccines are known to be less effective in people over 65. There is evidence that supplementing with DHEA before vaccination can improve antibody production to provide better protection.
https://my2048.com/product-category/dhea/
—–
-
Research News
The terms hyper-inflammation and cytokine storm are now part of the national lexicon, but most people still don’t understand the relationship between inflammation and immunity. We consider this must-have information because you will make important decisions during your life that depend on knowing:
- that early in infection, inflammatory proteins or cytokines help to activate the immune response.
- Left unchecked, however, these inflammatory cytokines start to damage healthy tissue. In Covid-19 infection, inflammation drives the fibrotic changes in the lungs that can take years to repair.
- A well-nourished body produces molecules that check inflammation at the appropriate stage of infection. They are called resolvins and protectins.
Picture General Resolvin and Colonel Protectin reviewing the immune cell troops.
General Resolvin: “First, I want to thank you for your extraordinary courage. What a battle, eh? Whew! So let’s have a moment of silence to remember our 487 billion comrades who were lost to this infection.”
Colonel Protectin: “And now that the battle is over, we want you to put down your weapons… That’s right; just put them in a pile over there in the lymph nodes. And then go home and relax. We’ll let you know when we need you again.”
So now, you’re eager to know where the resolvins and protectins come from. Because they’re absolutely needed for the resolution of any serious infection.
{drum roll}
Omega-3 fatty acids, mostly EPA and DHA.
For most people, the easiest way to optimize these critical molecules is to supplement with fish oil. Alternatives include krill oil and omega-3’s from algae. The liver can also convert alpha-linolenic acid (from seed and bean oils) to EPA, but this conversion is unreliable and declines with advancing age.
Action Step
Our Icelandic Omega-3 Fish Oil provides 900 mg of EPA and 600 mg of DHA per 3 capsule dose. Guaranteed to be free of mercury and PCB’s, and the best price available anywhere. A bottle of 90 capsules is $24.50/ Member price: $22.00. In a two-pack, it’s $45 with Member price: $39.95.
https://my2048.com/product-category/fish-oil/
For Members: https://thehealthyskeptics.com/product-category/fish-oil/
Please see pivotal reference (with abstract) at the end of this newsletter
——
-
Side note on insanity
Inflammation plays a critical role in diseases like psoriasis. So the Pharma answer is to develop monoclonal antibody (MAB) drugs to treat these diseases. These MABS completely suppress certain inflammatory cytokines, resulting in better-looking skin. Knowing what you’ve learned so far, can you see why it seems insane that we keep seeing ads for these MABS right in the middle of news reports on Covid-19? In the adverse side effect disclosure, these ads even state clearly that taking their drug increases your risk for infection and possibly death.
Related question: Can omega-3 fatty acids help in the treatment of psoriasis?
Answer: Absolutely, but does your dermatologist know this?
REFS:
- J Am Coll Nutr. 2002 Dec;21(6):495-505. Omega-3 fatty acids in inflammation and autoimmune diseases. Artemis P Simopoulos
- Int J Mol Sci. 2020 Jan 23;21(3):741. Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases. Anamaria Balić, et al.
——
-
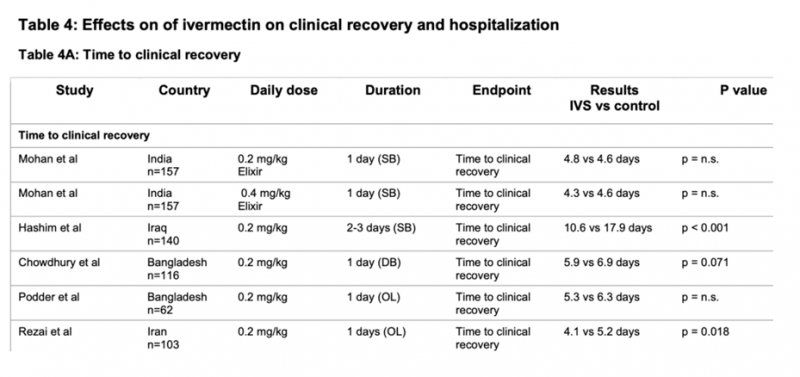
Ivermectin Update
Many of you are reporting that doctors are still not willing to write prescriptions for ivermectin; the most common reason being that the drug is not FDA approved to prevent or treat Covid-19.
Logical response:
“Well, doctor, I admit that there is no randomized, double blind human clinical trial to prove that ivermectin can prevent Covid-19 infection. But many doctors are taking it based on three observations:
- In countries where ivermectin is widely used to treat parasitic infections, the incidence of Covid-19 infection is remarkably low.
- There is a well-defined mode of action published in the medical literature:
REF: Antiviral Res. 2020 Jun;178:104787. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro
Leon Caly, et al.
- There are a growing number of published studies showing that the drug is effective in the early stages of Covid-19 infection. I just want to be prepared.
REFS:
- Efficacy of Ivermectin in COVID-19 Patients with Mild to Moderate Disease Karamat Hussain Shah Bukhari, et al.
Conclusion: In the Ivermectin arm, early viral clearance was observed and no side effects were documented. Therefore ivermectin is a potential addition to the standard care of treatment in COVID-19 patients.
Full text available at: https://www.medrxiv.org/content/10.1101/2021.02.02.21250840v1
- Rezai et al., IRCT20111224008507N3 (Preprint)
Effectiveness of Ivermectin in the Treatment of Coronavirus Infection in Patients admitted to Educational Hospitals of Mazandaran in 2020
—–
-
Pivotal references to read and share:
Fish oil
- Nutrition. 2021 Jan;81:110900. Parenteral fish oil: An adjuvant pharmacotherapy for coronavirus disease 2019?
Raquel S Torrinhas , Philip C Calder , Gabriela O Lemos , Dan L Waitzberg
Abstract
The new coronavirus associated with severe acute respiratory syndrome (SARS-CoV-2), surprisingly, does not affect only the lungs. The severe response to SARS-CoV-2 appears to include a “cytokine storm,” which indicates a state of hyperinflammation and subsequent dysfunction of multiple organs and tissues in the most severe cases. This could be the reason why populations at the highest risk for death from the SARS-CoV-2 infection-induced disease (coronavirus disease 2019 [COVID-19]) are those suffering from chronic low-grade inflammation, but prone to hyperinflammation. This includes individuals of advanced age and those with obesity, type 2 diabetes, hypertension, and metabolic syndrome. Inflammation resolution is strongly dependent on lipid mediators, the specialized pro-resolution mediators (SPMs). ω-3 polyunsaturated fatty acids (ω-3 PUFAs) are precursors of very potent SPMs, including resolvins, protectins, and maresins. Additionally, they are associated with a less aggressive inflammatory initiation, after competing with ω-6 fatty acids for eicosanoid synthesis. Therefore, it makes sense to consider the use of ω-3 PUFAs for clinical management of COVID-19 patients. ω-3 PUFAs may be given by oral, enteral, or parenteral routes; however, the parenteral route favors faster incorporation into plasma phospholipids, blood cells, and tissues. Here, we discuss these aspects to propose the parenteral infusion of ω-3 PUFAs as adjuvant immunopharmacotherapy for hospitalized patients with COVID-19.
Full text available at:
https://pubmed.ncbi.nlm.nih.gov/32738510/
—–
* DHEA:
This study explores the anti-inflammatory activity of DHEA and suggests that the decline of age-related immune competence (immunosenescence) is a direct result of decreased synthesis of DHEA (endocrinosenescence).
J Clin Endocrinol Metab. 1998 Jun;83(6):2012-7. doi: 10.1210/jcem.83.6.4876.
Serum DHEA and DHEA sulfate are negatively correlated with serum interleukin-6 (IL-6), and DHEA inhibits IL-6 secretion from mononuclear cells in man: possible link between endocrinosenescence and immunosenescence. R H Straub, et al
Full text available at:
https://pubmed.ncbi.nlm.nih.gov/9626133/
Thank you. Can you elaborate what the “legitimate reasons” to not get the vaccine are?
Since DHEA is helpful for immune competence, would pregnenolone also be of benefit?
I posted a question here yesterday but am not sure if it arrived. I wondered if Dr Natalie could elaborate on the legitimate reasons for not getting the vaccine. I am aware of allergic reactions in some people. What are the other reasons? Thank you.